Table of Contents:
- Understanding Different Types of Headaches
- Identifying Common Headache Triggers
- Effective Lifestyle Modifications
- Over-the-Counter Medications
- When to Seek Professional Help
- Alternative Therapies
- Preventive Medications
- Developing a Personalized Headache Management Plan
Understanding Different Types of Headaches
Millions of people experience headaches each year, but not all headaches are created equal. Recognizing the specific type you’re dealing with can be the first step toward effective relief. The three most common types are tension headaches, migraines, and cluster headaches. Tension headaches cause a dull ache across the forehead or neck, while migraines bring intense, throbbing pain that may be accompanied by nausea or sensitivity to light. Cluster headaches, though rare, are intensely painful and tend to occur in cycles, usually around one eye.
Because triggers and responses differ between headache types, understanding these differences is vital for preventative care. Identifying whether your symptoms point toward one variety over another can inform the strategies you use to minimize discomfort and avoid frequent recurrences. In some cases, issues such as constipation can contribute to headache frequency, underscoring the importance of a holistic approach to overall health.
Learning to differentiate your particular headache type empowers you to tailor management techniques for more successful relief. For example, a dull tension headache may respond well to lifestyle adjustments and relaxation, while migraines might require medication and a focus on trigger avoidance.
Less common cluster headaches usually call for specialized attention and sometimes even oxygen therapy for relief. When headaches occur regularly or disrupt your daily life, collaborating with a healthcare professional can clarify the underlying cause and lead to a more effective treatment strategy.
Identifying Common Headache Triggers
Understanding common triggers is essential for prevention. Everyday factors like heightened stress, inadequate hydration, and changes in sleep patterns can spark headaches. Skipping meals drops blood sugar and may set off discomfort, while consuming too much caffeine or alcohol can contribute to dehydration and pain. Bright lights or loud environments, especially for those prone to migraines, often serve as direct catalysts for symptoms. Keeping a headache diary can help identify personal patterns, which is an effective step toward minimizing episode frequency.
Effective Lifestyle Modifications
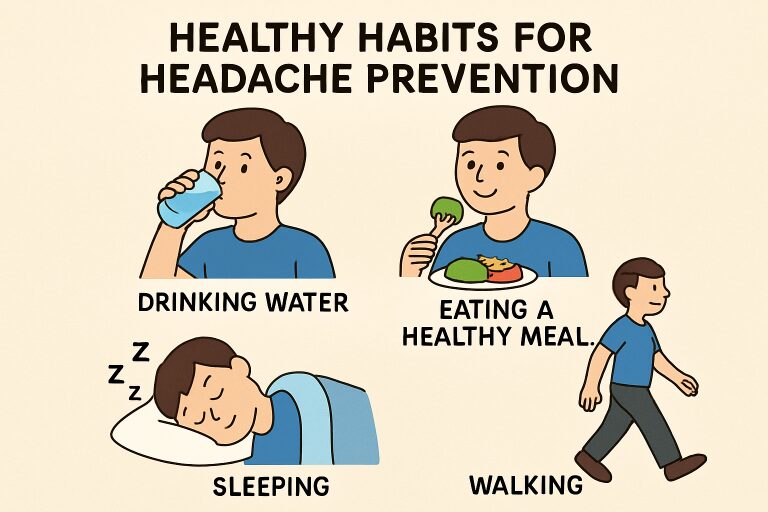
Proactive lifestyle changes can substantially reduce the burden of headaches. Maintaining a steady sleep schedule (aiming for 7 to 9 hours per night) provides your body with essential recovery. Hydration is equally important; adults should aim for at least eight cups of water daily to stave off dehydration-related headaches. Consuming a balanced diet, rich in whole foods and consistent meal times, stabilizes blood sugar and wards off hunger-triggered symptoms. Regular aerobic exercise, such as brisk walking, not only boosts overall well-being but can reduce stress—another potent headache trigger.
Alongside these approaches, stress management techniques like deep breathing, progressive muscle relaxation, and yoga offer natural support. Integrating these strategies into your routine can make a measurable difference in your headache frequency and intensity.
Over-the-Counter Medications
For occasional headaches, over-the-counter (OTC) medications provide quick, convenient relief. Common options include acetaminophen and NSAIDs such as ibuprofen, which can alleviate mild to moderate pain. Some formulations combine caffeine with pain relievers to boost their effects—a particularly effective strategy for some individuals. However, overuse of these products can backfire, upping the risk of rebound headaches and chronic symptoms. It’s crucial to follow label directions and avoid prolonged use without consulting a health professional.
When to Seek Professional Help
Knowing when a headache requires medical attention is critical. Frequent, severe, or worsening headaches, or those accompanied by neurological signs such as vision loss, confusion, or numbness, warrant prompt evaluation. Persistent headaches that affect your daily activities—or a sudden change in pattern—should be brought to a healthcare provider’s attention. In some cases, more advanced interventions, such as prescription medications or diagnostic testing, are necessary to uncover an underlying condition and prevent complications.
Alternative Therapies
Alternative or complementary treatments can provide extra relief for individuals seeking to reduce reliance on medication alone. Acupuncture is one such therapy with evidence supporting its role in reducing both the frequency and severity of headaches for some headache sufferers. Biofeedback uses monitoring devices and mental exercises to teach control over certain bodily functions, supporting pain management. Some people benefit from herbal supplements like magnesium or riboflavin—though consultation with a healthcare provider is essential before starting any new regimen to prevent interactions or side effects.
Preventive Medications
For people with persistent or chronic headaches, daily preventive medications might be necessary. Beta-blockers are often prescribed for migraine sufferers, helping to reduce both frequency and intensity. Certain types of antidepressants, especially those affecting serotonin pathways, may also block headache onset. Anticonvulsants like topiramate are another class that has shown effectiveness for some individuals. These medications must be used under a physician’s guidance, as they may require trial and adjustment to achieve the best results with minimum side effects.
Developing a Personalized Headache Management Plan
Since headache triggers and effective treatments vary widely from person to person, crafting a tailored management plan is crucial. Start by keeping a headache diary to log dates, symptoms, triggers, and relief strategies. Pair this with targeted lifestyle changes, focusing on hydration, diet, and sleep. Finally, work closely with your healthcare provider to adjust medications and therapies, ensuring a comprehensive, evolving plan that meets your needs. Consistency and patience are key; many people achieve significant improvement with perseverance and professional guidance.





